Sciatica: What That Shooting Leg Pain Really Means

If you’ve ever felt pain shooting from your lower back or buttock down your leg, you’ve likely experienced sciatica. Despite its name, sciatica isn’t a disease it’s a symptom that something is irritating or compressing the large sciatic nerve.
The key to relief is understanding what’s causing that nerve irritation and treating it directly not just masking the pain.
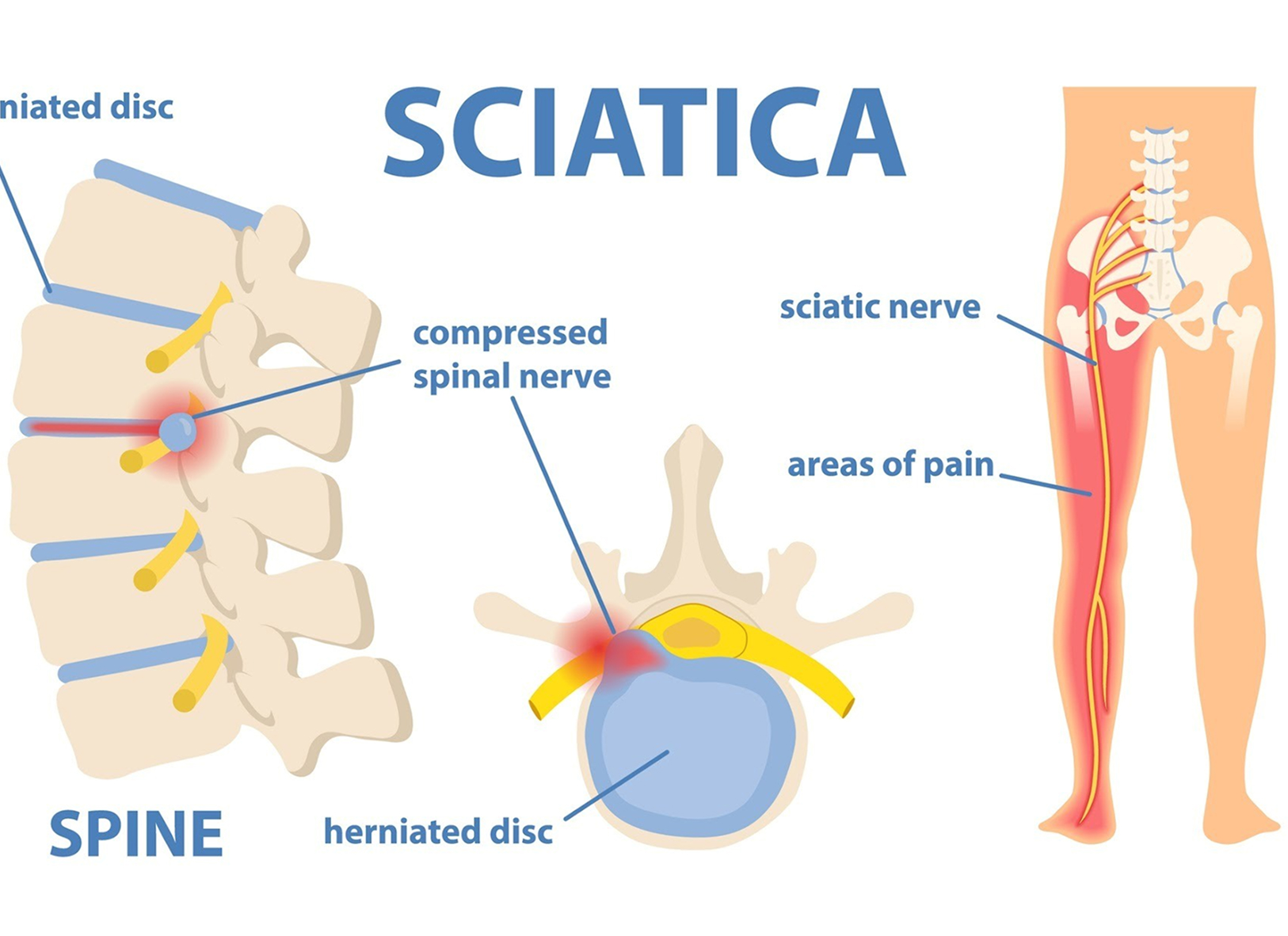
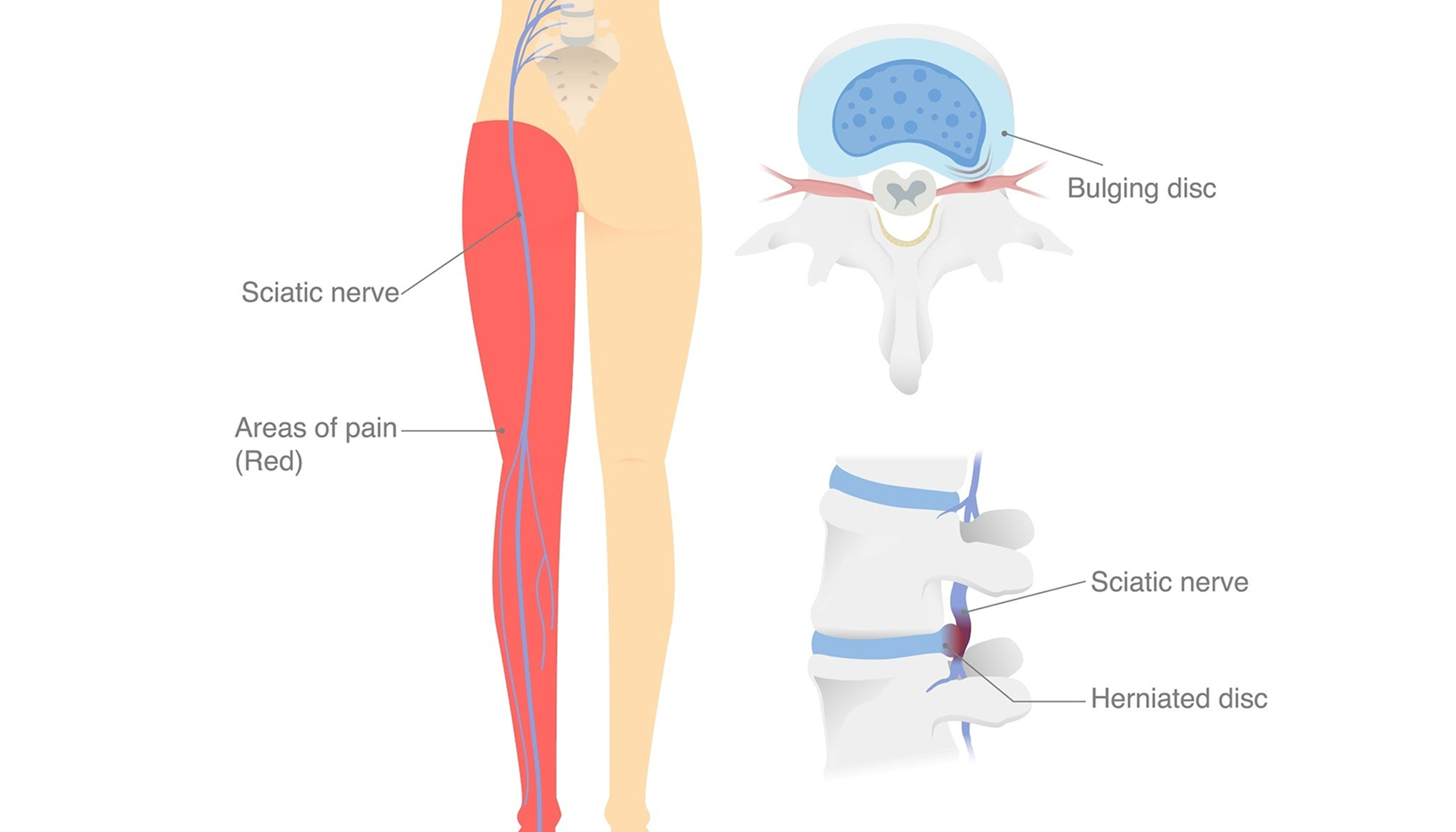
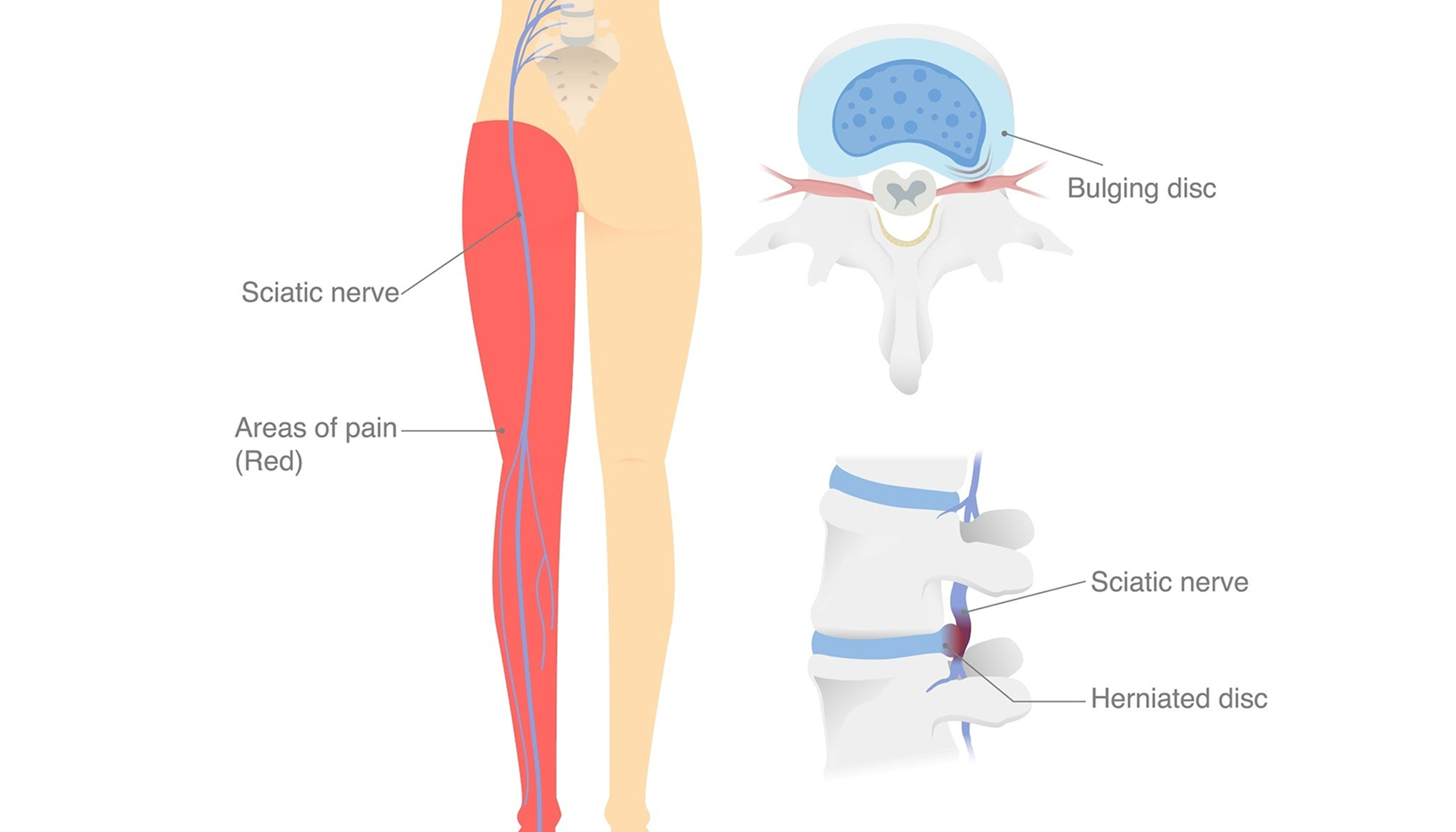
What Is the Sciatic Nerve?

The sciatic nerve is the body’s longest nerve. It begins in the lower spine, travels through the buttock, and runs down each leg. When any part of this nerve becomes compressed or inflamed, it can cause burning, tingling, or sharp pain that radiates down the leg.
Common Causes of Sciatica

Sciatica can result from several underlying issues. Identifying the correct cause helps target treatment precisely.

Bulging or Herniated - Disc A disc pressing on a nerve root.
Lumbar Spinal Stenosis - Narrowing of the spinal canal compressing the nerve.
Degenerative Disc Disease - Loss of disc height increasing nerve tension.
Spondylolisthesis - A vertebra slipping forward and pinching the nerve.
Piriformis Syndrome - A tight muscle in the buttock compressing the sciatic nerve.
Inflammation or Facet Arthropathy - Arthritic changes irritating nearby nerves.
What It Feels Like

Sciatic nerve pain can range from annoying to debilitating. Common symptoms include:
Shooting or burning pain down one leg
Numbness or tingling in the calf or foot
Weakness when standing or walking
Pain that worsens when sitting or coughing
These patterns help specialists identify the nerve root involved (L4, L5, or S1).
What It Feels Like

Sciatic nerve pain can range from annoying to debilitating. Common symptoms include:
Shooting or burning pain down one leg
Numbness or tingling in the calf or foot
Weakness when standing or walking
Pain that worsens when sitting or coughing
These patterns help specialists identify the nerve root involved (L4, L5, or S1).

When to Seek Medical Help

See a specialist if your pain lasts longer than a few days, or if it’s accompanied by:
Increasing weakness in the leg or foot
Numbness in the groin or saddle area
Loss of bladder or bowel control
Pain after trauma or infection
Prompt evaluation helps prevent permanent nerve damage.
How Sciatica Is Diagnosed

An accurate diagnosis starts with listening to your story, then confirming findings through:
Physical exam to identify pain distribution
Imaging (MRI or CT) to view discs, nerves, and bone alignment
Diagnostic nerve block to pinpoint the exact pain source
This approach ensures that treatment addresses the root cause not just symptoms.

When to Seek Medical Help

See a specialist if your pain lasts longer than a few days, or if it’s accompanied by:

Increasing weakness in the leg or foot
Numbness in the groin or saddle area
Loss of bladder or bowel control
Pain after trauma or infection
Prompt evaluation helps prevent permanent nerve damage.
How Sciatica Is Diagnosed

An accurate diagnosis starts with listening to your story, then confirming findings through:

Physical exam to identify pain distribution
Imaging (MRI or CT) to view discs, nerves, and bone alignment
Diagnostic nerve block to pinpoint the exact pain source
This approach ensures that treatment addresses the root cause not just symptoms.
Non-Surgical Treatment Options

Modern interventional pain care can often resolve sciatica without surgery.

Epidural Steroid Injection (ESI)
Delivers anti-inflammatory medication directly around the irritated nerve root to reduce swelling and pain.

Platelet-Rich Plasma (PRP) or Bone Marrow “Cell” Therapy
For disc or joint degeneration contributing to nerve compression, biologic injections can promote tissue repair.
What About Surgery?

Surgery is reserved for cases where conservative measures fail or there’s severe nerve compression causing progressive weakness or loss of function. Even then, minimally invasive spine specialists often achieve excellent outcomes without open surgery.
Get Back to Moving Comfortably
If you’re struggling with leg pain or numbness, don’t ignore it. Identifying and treating the cause early can prevent lasting damage and restore your quality of life.
© 2026 Elite Pain and Health. All Rights Reserved.



