Sacroiliitis: Inflammation of the Joint Connecting Your Spine and Pelvis

If you have deep pain in the lower back, buttock, or hip that worsens with standing or climbing stairs, the cause may be Sacroiliitis inflammation of the sacroiliac (SI) joint, where the spine meets the pelvis.
Because SI joint pain can mimic hip or lumbar spine issues, precise diagnosis is essential.
What Is the Sacroiliac Joint?

The sacroiliac joints sit on either side of the spine, connecting the sacrum
(the base of your spine) to the iliac bones of your pelvis.
These joints play a vital role in:
Transferring weight between the upper body and legs
Providing stability during walking or standing
Absorbing shock from movement
When irritated or inflamed, they can produce deep, localized pain that may radiate to the buttock or thigh.
What Causes Sacroiliitis


Arthritis or joint wear (degenerative sacroiliitis)
Inflammatory disease (such as ankylosing spondylitis)
Injury or trauma (falls, car accidents)
Pregnancy and childbirth (ligament stretching and pelvic stress)
Uneven leg length or posture imbalance
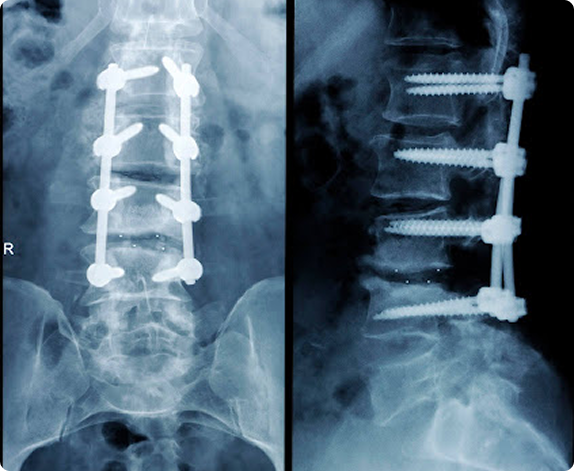
Previous lumbar fusion or surgery increasing SI joint load
Common Symptoms

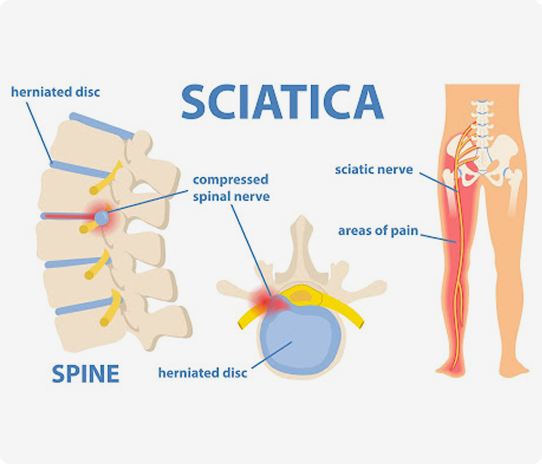
Sacroiliitis can cause pain patterns often confused with sciatica or hip disorders. Typical features include:
Deep aching pain in the lower back, buttock, or hip (often one-sided)
Pain that worsens with standing, stair climbing, or sitting for long periods
Discomfort rolling over in bed or getting out of a car
Occasional radiation of pain into the thigh (but rarely below the knee)

Common Symptoms

Sacroiliitis can cause pain patterns often confused with sciatica or hip disorders. Typical features include:

Deep aching pain in the lower back, buttock, or hip (often one-sided)
Pain that worsens with standing, stair climbing, or sitting for long periods
Discomfort rolling over in bed or getting out of a car
Occasional radiation of pain into the thigh (but rarely below the knee)
How It’s Diagnosed

Because SI joint pain can mimic other spine or hip problems, accurate diagnosis requires
a combination of clinical assessment and image-guided testing

Physical Examination
Special tests that stress the SI joint (e.g., FABER, Gaenslen, or compression tests) reproduce pain when the joint is inflamed.

Imaging
X-rays or MRI: reveal inflammation, arthritis, or joint changes.
CT Scan: may show bone irregularities or ankylosis in chronic cases.
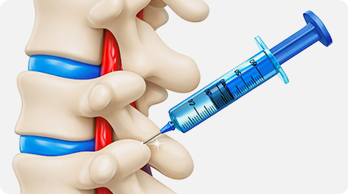
Diagnostic Nerve Block
An image-guided SI joint injection with numbing medication remains the gold standard for confirming the diagnosis—if the pain temporarily disappears, the joint is the source.
Risk Factors

Women during or after pregnancy
Individuals with prior lumbar fusion
People with autoimmune or inflammatory conditions
Athletes or laborers with repetitive pelvic stress
Those with leg length differences or scoliosis
Risk Factors

Women during or after pregnancy
Individuals with prior lumbar fusion
People with autoimmune or inflammatory conditions
Athletes or laborers with repetitive pelvic stress
Those with leg length differences or scoliosis
© 2026 Elite Pain and Health. All Rights Reserved.

