Lumbar Radiculopathy: When a Pinched Nerve Causes Leg Pain

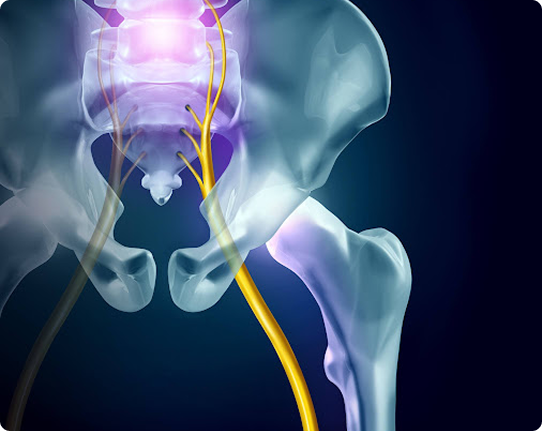
When a nerve root in your lower back becomes irritated or compressed, it can cause pain, tingling, numbness, or weakness that travels down your leg. This is called Lumbar Radiculopathy commonly referred to as a “pinched nerve.”
Understanding the anatomy and cause is essential to finding lasting relief.
What Is Lumbar Radiculopathy?

The lumbar spine contains nerve roots that branch off from the spinal cord and travel to your hips, legs, and feet. Each nerve root exits the spinal column through a small space between vertebrae called a foramen.
When that space narrows or a nearby disc or joint presses on the nerve, inflammation develops and signals pain along the nerve’s pathway.
Common Causes

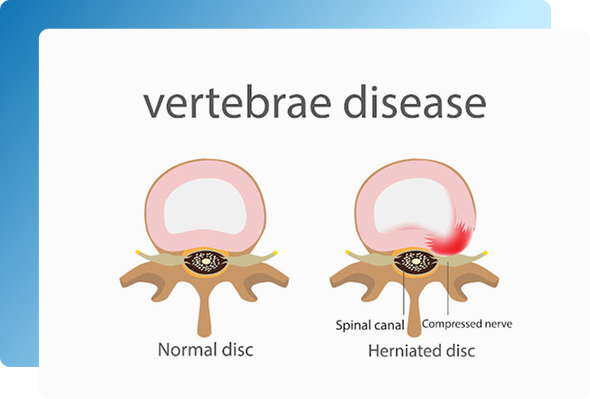
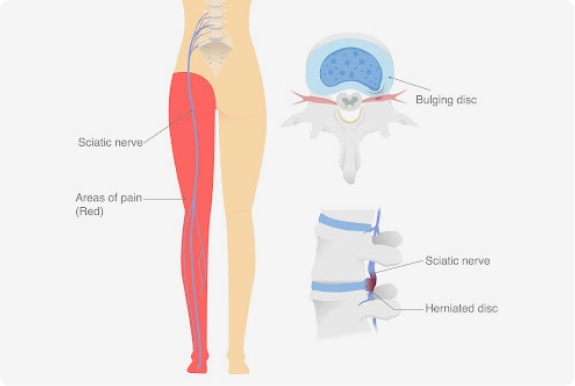
Herniated or Bulging Disc – Disc material protrudes and compresses a nerve root.
Degenerative Disc Disease – Disc height loss narrows the opening for the nerve.
Spinal Stenosis – Age-related narrowing of the spinal canal.
Spondylolisthesis – A vertebra slips forward, pinching the nerve.
Facet Joint or Bone Spur Formation – Arthritic changes encroach on the nerve space.
Common Symptoms

Low back or neck pain that worsens with sitting or bending
Pain that improves when walking or lying down
Occasional shooting or tingling sensation down the leg (if nerves are affected)
Stiffness, reduced flexibility, or pain after activity

Common Symptoms


Low back or neck pain that worsens with sitting or bending
Pain that improves when walking or lying down
Occasional shooting or tingling sensation down the leg (if nerves are affected)
Stiffness, reduced flexibility, or pain after activity

Who Is at Risk

Middle-aged adults (30–60 years old)
Individuals performing heavy lifting or twisting
Those with prior spinal degeneration or injury
People with sedentary or desk-bound jobs
Who Is at Risk


Middle-aged adults (30–60 years old)
Individuals performing heavy lifting or twisting
Those with prior spinal degeneration or injury
People with sedentary or desk-bound jobs
Symptoms

Other common symptoms include:
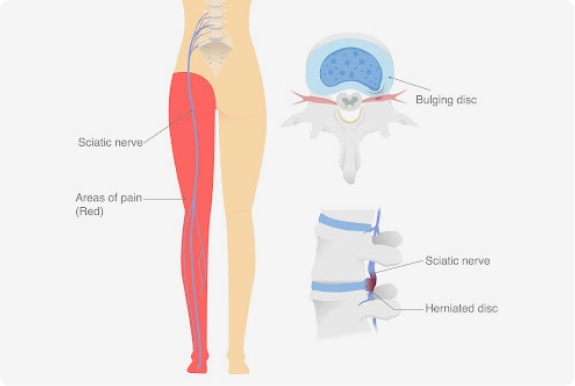
Shooting or burning pain down the leg
Numbness or tingling in a specific area
Muscle weakness or loss of reflexes
Pain that worsens with sitting, coughing, or sneezing

When to Seek Medical Attention

You should see a specialist if:
Pain lasts longer than 1–2 weeks despite rest
Weakness, numbness, or tingling develops
Pain radiates below the knee or into the foot
You experience loss of bladder or bowel control (emergency)
When to Seek Medical Attention

You should see a specialist if:

Pain lasts longer than 1–2 weeks despite rest
Weakness, numbness, or tingling develops
Pain radiates below the knee or into the foot
You experience loss of bladder or bowel control (emergency)
How It’s Diagnosed

Diagnosis starts with a detailed history and neurological exam. Specialists then use imaging and targeted diagnostic procedures to confirm which nerve is involved.

Physical Examination
Reflex testing, muscle strength assessment, and sensory mapping determine which nerve root may be affected.

Imaging
MRI: visualizes soft tissue and nerve compression.
CT or CT Myelogram: may be used if MRI is inconclusive.

Electrodiagnostic Testing (EMG/NCS)
Confirms nerve function and differentiates radiculopathy from peripheral neuropathy.
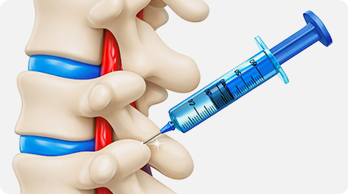
Diagnostic Nerve Block
A precise, image-guided injection of numbing medicine can confirm the source of pain.
© 2026 Elite Pain and Health. All Rights Reserved.

